Birth Control Options
This page lists all of the different types of birth control methods that are available in Canada. These methods vary in cost depending on region and coverage. For a look into estimated costs, check out our birth control cost chart here.
Hormonal Methods (Pill, Patch, Ring, Shot, IUD, Implant)
Non-Hormonal & Barrier Methods (Copper IUD, Condoms, Spermicides, Diaphragm, Cervical Cap, Sponge, Dental Dams & Gloves)
Other Methods (FABM, Withdrawal, Abstinence, Dual Protection, Emergency Birth Control, Postpartum Birth Control)
Permanent Methods / Sterilization (Tubal Ligation, Vasectomy)
Hormonal Birth Control Methods
- The Pill
- Seasonale/Seasonique
- The Mini Pill
- The Patch
- The Ring
- The Shot
- The IUS (Hormonal Implant)
- The Implant
Hormonal Oral Birth Control

How effective is this method?
- 92% with typical use
- 99.7% with perfect use
What is it?
- Small tablets that must be taken once a day, at the same time each day
- Contains two types of hormones: progestin and estrogen
- A pack can contain 21 pills (no sugar pills) or 28 pills (7 sugar pills)
- Sugar pills contain no hormones and act as a reminder to take your pill
- The pill is a reversible (non-permanent) method of contraception that is available in a variety of brands, strengths and formulas
How does it work?
- Prevents the ovary from releasing an egg
- Thickens cervical mucus to make it more difficult for a sperm to reach an egg
- Thins the lining of the uterus to make the implantation of an egg more difficult
Advantages |
Disadvantages |
|---|---|
| Doesn’t interfere with sexual activity | Must be taken every day at the same time |
| Regulates menstrual cycle | May cause irregular bleeding or spotting, breast tenderness, nausea or headaches |
| Reduces menstrual flow and cramps | May increase risk of blood clots |
| Decreases premenstrual symptoms, acne, and risk of endometrial and ovarian cancers | Effectiveness may be reduced by other medications |
| Not to be taken by people who cannot take estrogen, who are breastfeeding and/or are over age 35 who smoke |
Hormonal Continuous Oral Birth Control

How effective is this method?
- 92% with typical use
- 99.7% with perfect use
What is it?
- Similar to the birth control pill, this method has small tablets that must be taken once a day, at the same time
- Contains two types of hormones: progestin and estrogen
- Unlike the standard pill, where you take 21 active pills followed by sugar pills (or no pills at all) for 7 days, this method allows you to take the active (hormonal) pills for three months
- Every three months, one week of sugar pills are taken, during this time, you will get a menstrual period
- One period every three months means only four periods per year
- A pack contains 91 pills
- The pill is a reversible (non-permanent) method of contraception
How does it work?
- Prevents the ovary from releasing an egg
- Thickens cervical mucus to make it more difficult for a sperm to reach an egg
- Thins the lining of the uterus to make the implantation of an egg more difficult
Advantages |
Disadvantages |
|---|---|
| Must be taken every day at the same time | |
| Doesn’t interfere with sexual activity | More likely to have spotting or breakthrough bleeding than a 21 or 28 day pill |
| Regulates menstrual cycle | May increase risk of blood clots |
| Fewer periods; lighter flow | Effectiveness may be reduced by other medications |
| Pregnancy can be difficult to detect without a monthly period |
Hormonal Oral Birth Control: progestin-only

How effective is this method?
- 92% with typical use
- 99.7% with perfect use
What is it?
- Small tablets that must be taken once a day, at the same time
- Contains progestin only: no estrogen
- This pill is a reversible (non-permanent) method of contraception that is available only in packs of 28 days, with no hormone-free interval
How does it work?
- May inhibit the release of an egg
- Thickens cervical mucus to make it more difficult for a sperm to reach an egg
- Thins the lining of the uterus to make the implantation of an egg more difficult
Advantages |
Disadvantages |
|---|---|
| Doesn’t interfere with sexual activity | Must be taken every day at the same time |
| May reduce menstrual flow, cramps and premenstrual symptoms | may cause irregular bleeding or spotting, breast tenderness, abdominal bloating, acne or headaches |
| May be suitable for people who can't take estrogen, who are breastfeeding and/or are over age 35 who smoke | Effectiveness may be reduced by other medications |
Hormonal Transdermal Birth Control Patch (Evra)
How effective is this method?
- 92% with typical use
- 99.7% with perfect use
What is it?
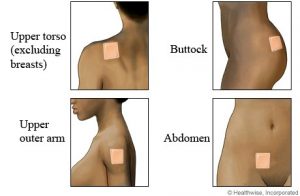
- A patch that slowly releases hormones (estrogen and progestin) through the skin
- The patch is a reversible (non-permanent) method of contraception; can be placed on buttocks, upper outer arms, lower abdomen or upper torso (not on breasts)
- New patch is applied once a week for three weeks, followed by one week without a patch
How does it work?
- Prevents the ovary from releasing an egg
- Thickens cervical mucus to make it more difficult for a sperm to reach an egg
- Thins the lining of the uterus to make the implantation of an egg more difficult
Advantages |
Disadvantages |
|---|---|
| No daily routine required (applied once-a-week) | May cause irregular bleeding or spotting, breast tenderness, nausea or headaches |
| Doesn’t interfere with sexual activity | Patch may detach from skin early and possible skin irritation at application site |
| Regulates menstrual cycle | May increase risk of blood clots |
| Reduces menstrual flow and cramps | Effectiveness may be reduced by other medications |
| Expected to provide similar non-birth control benefits to the pill, more research is needed | May not be suitable for people weighing over 198 pounds |
| Not to be taken by people who can’t take estrogen, who are breastfeeding and/or are over age 35 who smoke |
Hormonal Vaginal Birth Control Ring (NuvaRing)

How effective is this method?
- 92% with typical use
- 99.7% with perfect use
What is it?
- A flexible, nearly transparent, ring that is inserted into the vagina
- The ring is a reversible (non-permanent) method of contraception inserted into the vagina that releases a continuous dose of hormones (estrogen and progestin) for the three weeks, followed by one week without a ring
How does it work?
- Prevents the ovary from releasing an egg
- Thickens cervical mucus to make it more difficult for a sperm to reach an egg
- Thins the lining of the uterus to make the implantation of an egg more difficult
Hormonal Injectable Birth Control (Depo Provera)
How effective is this method?
- 97% with typical use
- 99.7% with perfect use
What is it?
- An injection which contains only progesterone (no estrogen)
- A reversible (non-permanent) method of contraception given by a health care provider in upper-arm or buttocks every 12-13 weeks (four times per year)
How does it work?
- Prevents the ovary from releasing an egg
- Thickens cervical mucus to make it more difficult for a sperm to reach an egg
- Thins the lining of the uterus to make the implantation of an egg more difficult
Advantages |
Disadvantages |
|---|---|
| No daily routine required (one injection 4 times/ year) | At first, irregular bleeding is quite common |
| Periods may stop: reported by over 50% after 1 year & more than 66% after 2 years | Causes a decrease in bone mineral density (may return to normal after stopping use) |
| Reduces: menstrual cramps, risk of endometrial cancer and frequency of epileptic seizures | May be connected to weight gain in some people |
| May improve symptoms of endometriosis, premenstrual syndrome and chronic pelvic pain | Can take 9 months or longer after last injection for ovaries to start releasing eggs again |
| Effectiveness not affected by most medications | Lack of monthly period may be bothersome for some |
| May be suitable for people who can’t take estrogen, who are breastfeeding and/or are over age 35 who smoke | Must be given by health-care professional |
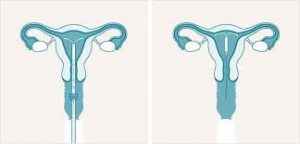
Hormonal Intrauterine System
How effective is this method?
- 99.8% with typical use
- 99.8% with perfect use
What is it?
- A small T-shaped device inserted into the uterus – brand names Mirena and Kayleena
- Contains hormone called levonorgestrel (a progestin, no estrogen) that is released slowly over time
- A long-acting reversible (non-permanent) method inserted by a health care provider that can remain in the uterus for 5 years
How does it work?
- Thickens cervical mucus making it more difficult for sperm to pass through cervix
- Thins the lining of the uterus to make the implantation of an egg more difficult
- Changes endometrial chemistry to decrease the sperm’s ability to fertilize an egg
- In some people, it may prevent the ovary from releasing an egg
Advantages |
Disadvantages |
|---|---|
| Long-acting method | May cause irregular bleeding/ spotting in first months after insertion |
| No routine needed | Perforation of uterus may occur at insertion (rare) |
| Doesn’t interfere with sexual activity | Insertion may be uncomfortable or painful |
| May reduce menstrual cramps, flow, pain due to endometriosis and the risk of endometrial cancer | May fall out of uterus (rare) |
| Some users may stop having menstrual cycles | Should not be inserted in people who have an active bacterial STI or pelvic infection |
| May be suitable for people who can’t take estrogen, who are breastfeeding and/or are over age 35 who smoke | Must be inserted and removed by health-care provider |
Etonogestrel implant 
How effective is this method?
- Over 99% with typical use
- Over 99% with perfect use
What is it?
- Hormone-releasing birth control implant
- Flexible plastic rod inserted under the skin of the inner side of upper arm (about the size of a matchstick)
- Contains a progestin hormone called etonogestrel
How does it work?
- Stops the release of an egg from the ovary
- Thickens cervical mucus in the cervix to keep sperm from reaching the egg
- Thickens lining of the uterus
Non-Hormonal & Barrier Methods
- The IUD
- External (Male) Condom
- Internal (Female) Condom
- Spermicides
- Diaphragm & Cervical Cap
- The Sponge
- Dental Dams & Gloves
Copper Intrauterine Device (No hormones)
How effective is this method?
- 99.1% with typical use
- 99.1% with perfect use
What is it?
- T-shaped device with a copper wire around it, inserted into the uterus
- A long-acting reversible (non-permanent) method inserted by a health care provider that can remain in uterus for 5 – 10 years
How does it work?
- Changes endometrial chemistry to decrease the sperm’s ability to fertilize an egg
- Decreases sperm’s ability to get through the cervical mucus
Advantages |
Disadvantages |
|---|---|
| Long-acting method | May cause irregular bleeding/ spotting in first months after insertion |
| No routine needed | May cause menstrual bleeding or cramping |
| Doesn’t interfere with sexual activity | Perforation of uterus may occur at insertion (rare) |
| May reduce risk of endometrial cancer | Insertion may be uncomfortable or painful |
| No hormones | May fall out of uterus (rare) |
| Should not be inserted in people who have an active bacterial STI or pelvic infection | |
| Must be inserted and removed by health-care provider |
How effective is this method? 
- 85% with typical use
- 98% with perfect use
What is it?
- A soft, disposable sheath that fits over an erect penis
- Reversible (non-permanent) method of birth control
- Comes in various shapes, sizes, thicknesses, colours and flavours
- Flavoured condoms are used for oral sex on a person with a penis
- Most are made of latex, but some are non-latex (often polyurethane)
How does it work?
- Fits over erect penis and acts as a physical barrier to prevent direct contact with vagina, anus or mouth; preventing exchange of bodily fluids
- Traps sperm in the condom so it cannot fertilize an egg
- The condom is thrown away in the garbage after sexual activity
- A new condom must be used for each new activity
Advantages |
Disadvantages |
|---|---|
| Inexpensive (can find for free) | Must be available at time of sexual activity |
| Protection against STIs | May reduce sexual spontaneity or sensitivity for either partner |
| Allows person with a penis to be responsible for birth control | Must be stored and handled properly |
| Both partners can participate in use | May slip or break during sexual activity |
| May help wearer avoid early ejaculation | May interfere with maintenance of an erection |
| No hormones | Condoms with spermicides should not be used as they irritate the vagina and anus and can increase contraction of HIV and STIs |
How effective is this method?
- 79% with typical use
- 95% with perfect use
What is it?
- A soft, disposable, polyurethane sheath that fits into the vagina
- Reversible (non-permanent) method of birth control
How does it work?
- Lines vagina or rectum completely, preventing direct contact with penis and prevents exchange of bodily fluids
- Traps sperm in condom so it cannot fertilize the egg
- Condom is thrown away in the garbage after sexual activity
- A new condom must be used for each new activity
Advantages |
Disadvantages |
|---|---|
| Used only at time of sexual activity | Must be available at time of sexual activity |
| Protection against STIs | May reduce sexual spontaneity or sensitivity for either partner |
| Person using it is in charge of placement and use | Requires proper insertion technique |
| Suitable for people with a latex allergy | Flexible inner ring may cause discomfort for some (can remove) |
| No hormones | May make a noise, slip or break during sexual activity |
| Difficult to use at first for some people, but becomes easier with practice |
How effective is this method?
- 71% with typical use
- 82% with perfect use
What is it?
- Chemical agent that affects sperm mobility and life
- Reversible (non-permanent) method of birth control
- Spermicides come in several forms: creams, jellies, tablets, suppositories, foams and film
How does it work?
- Inserted into the vagina up to 1 hour before sexual activity
- Affects sperm mobility and life
- Should be used with other birth control methods
- Vagina cannot be rinsed/washed for specific amount of time after sexual activity (varies based on type and brand)
Advantages |
Disadvantages |
|---|---|
| Used only at time of sexual activity | Must be available at time of sexual activity |
| Person using it is in charge of placement and use | Spermicide must be inserted into vagina in advance (depends on product) |
| Spermicide may provide added lubrication | Vagina must not be washed for specific time frame after sex |
| No hormones | Use of spermicide can cause irritation of vaginal and rectal walls increasing risk of contracting HIV and STIs |
| Cannot be used by people with spermicide allergies or sensitivities |
 How effective is this method?
How effective is this method?
|
Diaphragm |
Cervical Cap |
| 84% with typical use94% with perfect use | 40-60% with typical use74-91% with perfect use |
What is it?
- Intravaginal barrier methods used together with spermicide
- Diaphragm is a latex or silicone dome with flexible steel ring around edge
- Cervical cap is a thimble-shaped silicone cap
- Reversible (non-permanent) method of birth control positioned in vagina, over the cervix before sexual activity
How does it work?
- When positioned properly, they block entry by the sperm into the cervix
- Must be left in vagina for 6-8 hours after sexual activity
- Spermicide should be reapplied in the vagina for each repeated act of intercourse
Advantages |
Disadvantages |
|---|---|
| Used only at time of sexual activity | Must be available at time of sexual activity |
| Person using it is in charge of placement and use | Requires proper insertion technique |
| No hormones | Diaphragm may increase risk of persistent urinary tract infection |
| Use of spermicide can cause irritation of vaginal and rectal walls increasing risk of contracting HIV and STIs | |
| Cannot be used by people with spermicide allergies or sensitivities | |
| Cervical cap shouldn’t be used during menstruation – may cause vaginal odour and discharge | |
| May become dislodged during sexual activity | |
| If left in vagina longer than recommended, Toxic Shock Syndrome may occur |
How effective is this method?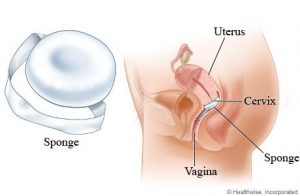
- 68% with typical use
- 80% with perfect use
What is it?
- The sponge is a soft disposable polyurethane device that is soaked in spermicide and bought at a pharmacy
- Reversible (non-permanent) method of birth control
How does it work?
- Inserted into vagina over cervix
- Effective for up to 12 hours
- Traps and absorbs sperm to prevent sperm from entering the cervix
Advantages |
Disadvantages |
|---|---|
| Used only at time of sexual activity | Must be available at time of sexual activity |
| Person using it is in charge of placement and use | Requires proper insertion technique |
| Spermicide may provide added lubrication | Spermicide must be inserted into the vagina in advance |
| No hormones | Use of spermicide can cause irritation of vaginal and rectal walls increasing risk of contracting HIV and STIs |
| Can't be used by people with spermicide allergies or sensitivities | |
| If left in vagina longer than recommended, Toxic Shock Syndrome may occur |
These are barrier methods that help protect against sexually transmitted infections (STIs). They do not prevent pregnancy.

What is it?
- Dental Dam: A soft, disposable latex, or non-latex, sheet that covers the vulva and/or anus to prevent fluid exchange and skin to skin contact
- Glove: Soft disposable latex, or non-latex material that covers the hand to block fluid exchange and skin to skin contact
How does it work?
|
Dental Dam |
Gloves |
|
Prevents fluids from being exchanged from mouth to vagina or anusA new dam must be used for each new activity or body part Lays on top of vulva or anus Dam is thrown away after sexual activity |
Covers hand(s) during sexual activity or can be cut open to act as a dental damPrevents fluids from being exchanged from mouth to vagina and/or anus A new glove must be used for each new activity or body part Glove is thrown away after sexual activity |
Advantages |
Disadvantages |
|---|---|
| Used only at time of sexual activity | Must be available at time of sexual activity |
| Partners can negotiate use and placement together | May reduce sexual spontaneity or sensitivity for either partner |
| Suitable for people with a latex allergy | May slip or break during sexual activity (especially if teeth are used) |
| No hormones | Difficult to use at first for some people, but becomes easier with practice |
| Protects against STIs |
Other Methods
- Fertility Awareness Based Methods (FABM)
- Withdrawal
- Abstinence
- Dual Protection
- Emergency Contraception
- Postpartum Birth Control
- Breastfeeding/Chestfeeding
How effective is this method? 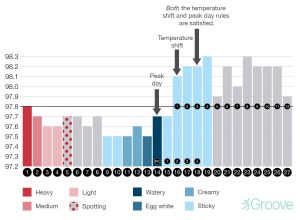
- 80% with typical use
- 91-99% with perfect use
What is it?
- A person who menstruates tracks the following to identify when they are, and are not, fertile:
- When they menstruate (track on a calendar)
- Cervical fluid (texture, amount, colour)
- Basal body temperature (first thing in the morning – looking for a spike in temperature that lasts a couple of days which shows ovulation)
- Symptoms and life stressors that may delay ovulation
How does it work?
- This information, when tracked properly will help a person understand when they are most likely to get pregnant after engaging in unprotected sex, and when they are most likely not to get pregnant after engaging in unprotected sex
- During the fertility period abstinence or another form of birth control must be used in order for the method to work effectively
Advantages |
Disadvantages |
|---|---|
| Allows the person with the uterus to understand their cycle and body | Demands motivation, willingness |
| The information on fertility may help with pregnancy planning | Requires a period of abstinence or use of another form of birth control |
| Cost-effective | Requires time and effort to learn the correct use of the method |
| No hormones | May affect sexual spontaneity |
How effective is this method?
- 73% with typical use
- 96% with perfect use
What is it?
- During sexual activity, a person with a penis must remove their penis from the vagina before ejaculation
- Ejaculation should not occur on the vulva or anus
How does it work?
- The penis is removed from the vagina before any sperm is released inside
- Ejaculation should occur away from the vagina as sperm on the vulva or anus can get into the vagina
- Most common problem with withdrawal is that the penis is withdrawn too late or the pre-ejaculate contained sperm
Advantages |
Disadvantages |
|---|---|
| May be used if other methods of contraception are not available at time of sexual activity | Requires a lot of self-control and practice |
| Can be used at the same time as any other method | Has a high failure rate |
| No hormones | Pre-ejaculate (drop of clear fluid on the tip of the penis when the penis is erect) may contain sperm and sexually transmitted infections |
| Cost-effective | May reduce pleasure for either partner |
| Allows person with penis to assume some responsibility for birth control |
Abstinence is the only 100% effective method of preventing pregnancy and sexually transmitted infections (STIs). Abstinence involves the decision to refrain from sexual activity (meaning no birth control is needed). Abstinence might have different definitions for different people and should be a topic of open communication between partners. People who choose abstinence will choose to avoid some or all of the following activities:
- Vaginal intercourse (penis in vagina sex)
- Oral sex (mouth to penis, vagina and/or anus)
- Anal intercourse (penis in anus sex)
- Genital contact (any type of direct touching of penis, vagina or anus)
- Penetration of vagina and/or anus by a sex toy
It is important to remember that if your definition of abstinence does not include all of these activities you may be at risk of unintended pregnancy and you are at risk of contracting a sexually transmitted infection (STI).
Dual protection refers to using more than one form of birth control at the same time to decrease the potential of a pregnancy or STI transmission (e.g. using a condom and the pill; using the ring and withdrawal; using the patch and a diaphragm). You cannot take more than one hormonal method at one time. Withdrawal can always be used with another method.
Emergency Contraception (EC) can help prevent pregnancy if used as soon as possible (from immediately to within 120 hours) after unprotected sex, birth control failure, or non-consensual sex. The effectiveness decreases with time. The two options for emergency contraception are Emergency Contraception Pills (ECP) and an Intrauterine Device (IUD).
Emergency Contraception Pills
Common brand names of Emergency Contraception Pills (ECPs) include “Plan B” “Next Choice” or “Ella.” All work similarly to the birth control pill by preventing ovulation, thickening cervical fluid and thinning the lining of the uterus. Plan B and Next Choice are over-the-counter medications, no prescription is needed to buy it. They may be on a shelf or behind the pharmacy counter. The cost ranges from $21 – $45 depending on where you go and what brand you buy. A prescription is necessary for Ella and it is effective for people with higher BMIs where Plan B and Next Choice are not.
These are some situations where ECP can be used:
- No birth control was used
- Missed birth control pills, patch or ring
- The condom broke, leaked or fell off inside or close to the vagina
- The diaphragm or cervical cap was dislodged or removed too early
- An error was made in a Fertility Awareness Based Method
- Non-consensual sex (sexual assault)
Intrauterine Device (IUD)
An IUD can be inserted by a health care provider into the uterus within 5 days of unprotected sex or birth control failure to prevent pregnancy. Your health care provider will review which IUD option is best for you. Getting an IUD may be difficult as it can be costly and it may be challenging to get an appointment with a health care provider within the short time frame required for it to be effective.
If you choose to use birth control after giving birth:
For the first 6 weeks after giving birth you will need to use non-hormonal methods of birth control such as:
- Condoms (external or internal)
- Diaphragm, cervical cap, sponge or spermicides
- Non-hormonal IUD
- Withdrawal Method
- Fertility Awareness Based Methods
After 6 weeks you can use hormonal methods of birth control. What types you can use will be different if you are breastfeeding/chestfeeding or bottle feeding.
If breastfeeding/chestfeeding you can use the following methods after 6 weeks:
- The mini pill
- The shot (Depo-Provera)
- IUD with hormones (IUS)
- Emergency Contraception
If bottle feeding you can use the above methods after 6 weeks plus:
- The pill
- The patch (Evra)
- The ring (NuvaRing)
Breastfeeding can be a form of birth control if done a certain way. When done properly breastfeeding is approximately as effective as using hormonal birth control. When you exclusively breastfeed – meaning you feed at least every 4 hours during the day and every 6 hours at night, and you feed your baby only breast milk – your body naturally stops ovulating. You can’t get pregnant if you don’t ovulate.
No ovulation also means no menstruation (period). Breastfeeding as birth control is also called the “lactational amenorrhea method (LAM).” Lactation refers to breastfeeding and amenorrhea refers to no period.
Breastfeeding will not prevent pregnancy if you feed your baby anything other than breastmilk. If you are also using formula this form of birth control is not recommended. It is also not recommended if you use a breast pump.
Breastfeeding can only be used for birth control for the first 6 months after birth or until your period returns. After this, breastfeeding is not an effective form of birth control, especially as the baby begins to eat solid foods and breastfeeds less frequently.
It is recommended to use a different type of birth control if: your period returns, your baby is 6 months old, you begin using formula, you start feeding your baby other food.
Permanent Methods (Sterilization)
How effective is this method?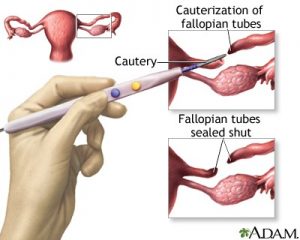
- 99.5% with typical use
- 99.5% with perfect use
What is it?
- Considered a permanent form of birth control
- A permanent surgical procedure to close or block the fallopian tubes:
- Laparoscopy: special instruments are inserted through two tiny incisions (less than 1 cm) in the abdomen
- Mini-laparotomy: small cut in abdomen (longer than 1 cm)
- Hysteroscopy: thin telescope inserted into uterus to see the opening of the fallopian tubes
How does it work?
- The fallopian tube is closed or blocked, meaning the sperm and egg can no longer meet
- Fallopian tubes can be closed or blocked with clip, ring, cauterization, or ligation
Advantages |
Disadvantages |
|---|---|
| No birth control routine needed | Usually permanent (difficult and expensive to reverse) |
| Doesn’t interfere with sexual activity | Possible short-term surgery complications: abdominal discomfort, bruising, bleeding, infection at the incision site or reaction to anesthesia |
| No significant long-term side effects | If pregnancy occurs, there is a higher chance for an ectopic pregnancy |
| No hormones | Failure rates vary depending on the type of procedure |
How effective is this method?
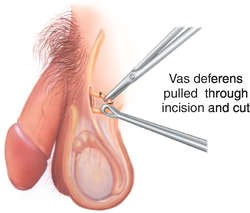
- 99.9% with typical use
- 99.9% with perfect use
What is it?
- A permanent surgical procedure to close or block the Vas Deferens (tubes that carry sperm to penis)
- An incision or puncture is made in the scrotum to reach the Vas Deferens
- Considered a permanent form of birth control
How does it work?
- The vas deferens are closed or blocked by cauterization, a clip, or the removal of a small segment of the tube so that sperm cannot be released during ejaculation
- Vasectomies do not interfere with erection, ejaculation or orgasm
- Sperm make up only 1% of the fluid ejaculated, ejaculation will look, smell and taste the same after a vasectomy
Advantages |
Disadvantages |
|---|---|
| No birth control routine required | Usually permanent procedure (difficult and expensive to reverse) |
| Doesn’t interfere with sexual activity | May regret having procedure in future |
| No significant long-term side effects | Possible short-term surgery complications: pain, vasovagal reaction, infection at incision site, bruising and swelling of the scrotum |
| Less invasive, fewer complications, and more cost-effective than tubal ligation (female) sterilization | Not effective immediately. Back-up contraception must be used between the time of surgery and the follow-up semen analysis to confirm that there is no sperm (2-3 months) |
| Allows person with penis to assume some responsibility for birth control |
Ready to Book an Appointment?
Current Wait Time: 2 weeks

